Prenatal diagnostic testing is used to determine whether your baby has a chromosomal abnormality. The most common types of prenatal diagnostic tests available are chorionic villus sampling (often simply called “CVS”) and amniocentesis (often simply called “amnio”).
At Advanced Women’s Imaging we are experienced at performing chorionic villus sampling (both the transabdominal and transvaginal approaches) and amniocentesis.
Chorionic villus sampling and amniocentesis are different from prenatal screening tests such as nuchal translucency scans.
Prenatal diagnostic testing is considered an invasive way of determining the presence or absence of a chromosome abnormality. These tests involve putting a needle into either the placenta or amniotic sac of the developing pregnancy and hence they are associated with an increased risk of miscarriage. These tests are usually performed only in certain situations.
Prenatal diagnostic testing (CVS and amniocentesis) provide a definitive (100%) diagnosis of a chromosome abnormality.
For example, CVS/amniocentesis will tell us either
- “no, the baby definitely does not have a chromosome abnormality”, or,
- “yes, the baby definitely has a chromosome abnormality”.
This is different from the results of combined first trimester screening (nuchal translucency scan and specific blood tests). First trimester screening is a “screening” test only and does not provide a definitive (100%) answer. First trimester screening simply tells us if the risk of your baby having a chromosome abnormality is high or low.
For example, first trimester screening will tell us either
- “the baby has a low risk of having trisomy 13,18 or 21”, or,
- “the baby has a high risk of having trisomy 13,18 or 21”.
First trimester screening gives us an indication of whether we should worry about your baby based on these results. If we are worried about your baby, prenatal diagnostic testing will be offered.
For more information about first trimester screening, please go to:
Nuchal translucency Ultrasound
CHORIONIC VILLUS SAMPLING
Not all women need prenatal diagnostic testing, including chorionic villus sampling.
Chorionic villus sampling may be suggested for a number of reasons including:
- Women over 35 years old.
- Women with “high risk” results on first trimester screening.
- Women with a history of chromosomal or genetic disorders.
- Women who prefer to have a definitive answer rather than a screening test.
The advantage of CVS compared to amniocentesis is that CVS is performed earlier. This means if results of the test are not normal, management of the pregnancy (such as curettage) may be less complicated.
The disadvantage of CVS compared to amniocentesis is that CVS is associated with a higher miscarriage rate (1 in 500 with CVS compared with 1 in 1000 with amniocentesis).
The advantage of CVS compared with first trimester screening is that CVS gives a definitive result, rather than just categorising your baby as high or low risk.
The disadvantage of CVS compared with first trimester screening is that CVS is associated with an increased risk of miscarriage due to the procedure.
- The dates/gestation of the pregnancy.
- The presence of baby’s heart beat.
- The number of babies.
- The position of the placenta and uterus.
- The basic structure of baby (for example, baby’s head and limbs).
- Transabdominal CVS This type of CVS is performed through the abdomen. The skin is cleansed with antiseptic solution and a sterile drape is placed over the abdomen. A small amount of local anaesthetic is injected into the skin and abdominal wall. A fine needle is passed through the mother’s abdominal wall into the developing placenta, under ultrasound guidance. A syringe attached to the end of the needle is then used to gently suction up a tiny amount of placenta (chorionic villi). When the CVS is finished, we will check the baby’s heart beat again to ensure all is well with baby. Most women experience some discomfort during transabdominal CVS, but this discomfort is not usually severe. The local anaesthetic used during this test helps decrease the discomfort but it does not eliminate discomfort completely.
- Transvaginal CVS This type of CVS is performed through the mother’s vagina/cervix. A speculum (like that used for pap smears) is placed into the vagina and the cervix visualised. The cervix is cleansed with antiseptic solution. A thin intrauterine catheter passes through the cervix into the uterus and developing placenta, under ultrasound guidance. A syringe attached to the end of the catheter is then used to gently suction up a tiny amount of placenta (chorionic villi). When the CVS is finished, we will check the baby’s heart beat again to ensure all is well with baby. Most women experience some discomfort during transvaginal CVS, but this is not usually severe. Some of this discomfort may be due to the bladder, which remains partially filled during this test.
The type of CVS you have depends largely on the position of the placenta. Both types of CVS are performed under constant ultrasound guidance, to ensure that the developing baby is not harmed.
We usually get better images during transabdominal ultrasound if the bladder is partially filled, so to help your examination we ask you to drink water prior to the assessment. Please empty your bladder 1 hour before your appointment, drink 2 glasses of water and try not to empty your bladder again until after your appointment.
A full bladder moves bowel out from the pelvis into the abdomen, helping visualisation of the pregnancy, uterus and cervix.
Your bladder should not be so full that it causes pain. If your bladder is very full and painful, you should empty a small amount so you are more comfortable.
Women that have a Rhesus negative blood group (for example, A Negative, O Negative) will receive an injection of anti-D immunoglobulin after the procedure. This is to prevent the mother from forming antibodies to the baby’s blood if the baby happens to have a Rhesus positive blood group.
If your blood group is written on your antenatal card, then just bring this card to your appointment.
Chorionic villus sampling is an invasive procedure. It is associated with an increased risk of miscarriage. This risk is approximately 1 in 500).
This procedure-related risk of miscarriage is the risk of miscarriage above the background rate of miscarriage. Miscarriage in the first trimester also occurs in women who have not had a CVS (called the background rate of miscarriage) and it is not uncommon.
Miscarriage is most likely to occur in the first 1-14 days after the procedure.
There is not usually a particular reason that miscarriage occurs following CVS, although it may be related to bleeding or infection.
You should call our practice or your referring doctor immediately if you have any of the following symptoms:
- Severe abdominal pain and/or increasing pain.
- Abnormal vaginal fluid loss.
- Heavy vaginal bleeding.
- Unexplained fever.
- Generally feeling unwell.
These symptoms may indicate a problem such as impending miscarriage or infection.
It is normal to have some discomfort following your CVS. This discomfort may feel like mild period cramping. This pain may persist for a few days and should gradually decrease in severity. Most women are able to drive after the test, but it is suggested that you bring a family member or friend to drive you home if possible. It is best to take the day off work.
You can use panadol for pain, if required. Aspirin in pregnancy should be avoided.
You may experience some vaginal bleeding after a CVS, especially if you had a transvaginal CVS. This bleeding or brown discharge may persist for a few days and should gradually decrease in severity.
Most CVS results are available within 10-14 days. It takes time for the laboratory to culture (grow) the chorionic villi and examine the chromosomes. This final result (long-term culture) examines all the baby’s chromosomes. If you requested rapid FISH testing (fluorescent in-situ hybridisation), this initial result is usually available within 48 hours. Rapid FISH testing only examines chromosomes 13, 18, 21 and the sex chromosomes (X and Y). These are the most common abnormal chromosomes.
A normal FISH result provides rapid reassurance for parents, especially if there is anxiety due to a high risk result on combined first trimester screening or an abnormal ultrasound. This rapid result does require confirmation with the long-term culture, which is more reliable. A normal FISH result is reassuring but it does not exclude all chromosome abnormalities. Our ultrasound doctor can phone you with the results. Alternatively, you can make an appointment to come into the practice to discuss your results in person, or you may choose to see your referring doctor to discuss the results. If there is a problem with your results, your referring doctor will be contacted directly.
Very occasionally, the CVS specimen fails to grow in the laboratory, or the results of the CVS are uncertain. If this occurs, you will still have the option of an amniocentesis at 15 weeks gestation. The amniocentesis gives us the same information about your baby’s chromosomes.
Most women will have normal results on their CVS (a baby with normal chromosomes).
Some women, however, will have abnormal results on their CVS (a baby with abnormal chromosomes) and require further counselling and management.
Abnormalities on CVS include extra chromosomes (such as trisomy 21 or Down syndrome), missing chromosomes (such as 45, X0 or Turner syndrome), deletions of portions of chromosomes, or re-arrangements of chromosomes (such as translocations). Chromosome abnormalities are often associated with structural problems in the baby.
We understand that abnormal results cause a great deal of anxiety and stress. You will have the opportunity to discuss your results with our ultrasound doctor. You may also wish to have further counselling with a geneticist or genetic counsellor, who specialise in this area of chromosome abnormalities. Making decisions about your baby can be extremely difficult. We will give you information and support, to help you during this difficult time.
Some women have a CVS because of a problem seen on ultrasound (for example, an increased nuchal translucency measurement). Having normal chromosomes on CVS will be reassuring, but it may be just one part of investigating your baby for possible problems. There may still be concerns of other conditions affecting the baby.
For example, the risk of heart defects is increased when the nuchal translucency measurement is very thick.
The doctor will discuss the need for any further tests with you. These tests may include a detailed 18-20 week morphology ultrasound and a fetal echocardiogram (a specialised heart ultrasound of the baby).
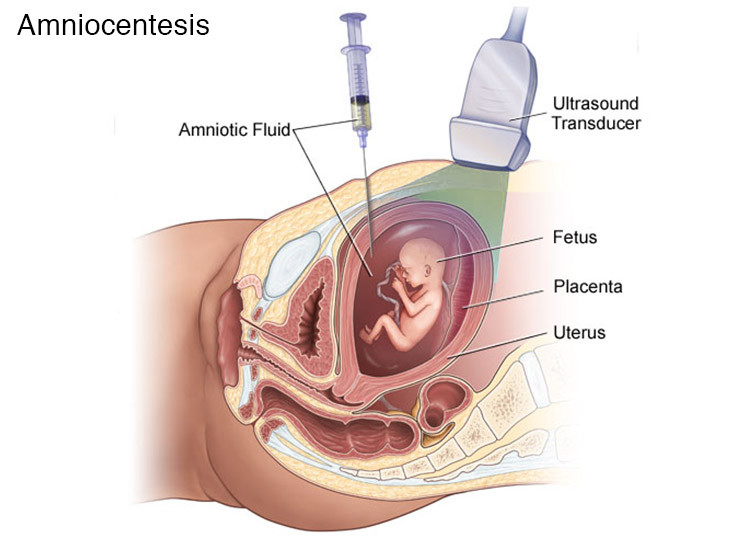
AMNIOCENTESIS
Amniocentesis is a prenatal diagnostic test usually performed around 15 weeks gestation onwards. . It involves passing a fine needle through the maternal abdomen into the amniotic sac (fluid around the baby) to obtain a small amount of amniotic fluid. This fluid contains cells from the baby that can be examined for their chromosomes. These cells are shed from the baby’s skin, lungs and bladder.
Not all women need prenatal diagnosis or amniocentesis.
Amniocentesis may be suggested for a number of reasons including:
- Women over 35 years old.
- Women with “high risk” results on first trimester screening.
- Women with a history of chromosomal or genetic disorders.
- Women who prefer to have a definitive answer rather than a screening test.
The advantage of amniocentesis compared to CVS is that amniocentesis is safer and associated with a lower miscarriage rate (1 in 1000 with amniocentesis compared with 1 in 500 with CVS).
The disadvantage of amniocentesis compared to CVS is that amniocentesis is performed later, so if results of the test are not normal, management of the pregnancy may be different.
The advantage of amniocentesis compared with first trimester screening is that amniocentesis gives a definitive result, rather than just categorising high or low risk women.
The disadvantage of amniocentesis compared with first trimester screening is that amniocentesis is associated with an increased risk of miscarriage.
Before your amniocentesis is performed, we will perform a transabdominal ultrasound.
The ultrasound will look mainly at:
- The dates/gestation of the pregnancy.
- The presence of baby’s heart beat.
- The number of babies.
- The basic structure of baby (for example, baby’s head and limbs).
- The position of the placenta.
- The location of the amniotic fluid to be sampled.
Amniocentesis is performed through the mother’s abdomen.
The skin is cleansed with antiseptic solution and a sterile drape is placed over the abdomen.
A fine needle is then passed through the mother’s abdominal wall into the amniotic sac, under ultrasound guidance. A syringe attached to the end of the needle is then used to gently withdraw a small amount of amniotic fluid (15-20ml). Amniotic fluid is mainly made up of baby’s urine. The baby quickly replaces this amniotic fluid over the next day.
When the amniocentesis is finished, we will check the baby’s heart beat again to ensure all is well with baby.
Most women experience some discomfort during amniocentesis but this discomfort is usually minimal. We do not use local anaesthetic or other analgesia during the test.
We usually get better images during transabdominal ultrasound if the bladder is partially filled, so to help your examination we ask you to drink water prior to the assessment. Please empty your bladder 1 hour before your appointment, drink 1-2 glasses of water and try not to empty your bladder again until after your appointment.
A full bladder moves bowel out from the pelvis into the abdomen, helping visualisation of the pregnancy, uterus and cervix.
Your bladder should not be so full that it causes pain. If your bladder is very full and painful, you should empty a small amount so you are more comfortable.
You will be able to empty your bladder completely once the transabdominal ultrasound is completed and before the amniocentesis is started.
Women that have a Rhesus negative blood group (for example, A Negative, O Negative) will receive an injection of anti-D after the procedure. This is to prevent the mother from forming antibodies to the baby’s blood if the baby happens to have a Rhesus positive blood group.
If your blood group is written on your antenatal card, then just bring this card to your appointment.
Amniocentesis is an invasive procedure and it is associated with an increased risk of miscarriage. This risk is low – approximately 1 in 1000).
This procedure-related risk of miscarriage is the risk of miscarriage above the background rate of miscarriage. Miscarriage in the first trimester also occurs in women who have not had an amniocentesis (called the background rate) and it is not uncommon.
A few percent of women have some leakage of amniotic fluid from the vagina, usually within the first 24-48 hours following amniocentesis. This leakage is usually transient and resolves without treatment. You should however let us know if this occurs.
You should call our practice or your referring doctor immediately if you have any of the following symptoms:
- Severe abdominal pain and/or increasing pain.
- Abnormal vaginal fluid loss.
- Heavy vaginal bleeding.
- Unexplained fever.
- Generally feeling unwell.
These symptoms may indicate a problem such as impending miscarriage or infection.
You should take it easy for the next 2 days. You do not need to stay in bed but you should avoid any strenuous exercise or heavy lifting. This includes lifting small children, carrying shopping bags and house cleaning or vacuuming.
It is normal to have some discomfort following your amniocentesis. This discomfort may feel like mild period cramping. This pain may persist for a few days and should gradually decrease in severity. Most women are able to drive after an amniocentesis, but it is suggested that you bring a family member or friend to drive you home if possible.It is best to take the day off work.
You should not have any bleeding or vaginal fluid loss.
You can use panadol for pain, if required. Aspirin should be avoided in pregnancy.
Most amniocentesis results are available within 2 weeks.
It takes time for the laboratory to culture (grow) the baby’s cells and examine the chromosomes. This final result (long-term culture) examines all the baby’s chromosomes. If you also requested rapid FISH testing (fluorescent in-situ hybridisation), this initial result is usually available within 48 hours.
Rapid FISH testing only examines chromosomes 13, 18, 21 and the sex chromosomes (X and Y). These are the most common abnormal chromosomes.
A normal FISH result provides rapid reassurance for parents, especially if there is anxiety due to a high risk result after combined first trimester screening or an abnormal ultrasound. This rapid result does require confirmation on the long-term culture, which is more reliable. A normal FISH result is reassuring but it does not exclude all chromosome abnormalities.
Our ultrasound doctor can phone you with the results. Alternatively, you can make an appointment to come into the practice to discuss your results in person, or you may choose to go back to your referring doctor to discuss the results. If there is a problem with your results, your referring doctor will be contacted directly.
Most women will have normal results on their amniocentesis (a baby with normal chromosomes).
Some women, however, will have abnormal results on their amniocentesis (a baby with abnormal chromosomes) and require further counselling and management.
Abnormalities on amniocentesis include extra chromosomes (such as trisomy 21 or Down syndrome), missing chromosomes (such as 45, X0 or Turner syndrome), deletions of portions of chromosomes, or re-arrangements of chromosomes (such as translocations). Chromosome abnormalities are often associated with structural problems in the baby.
We understand that abnormal results cause a great deal of anxiety and stress. You will have the opportunity to discuss your results with our ultrasound doctor. You may also wish to have further counselling with a geneticist or genetic counsellor, who specialise in this area of chromosome abnormalities.
Making decisions about your baby can be extremely difficult. We will give you information and support, to help you during this difficult time.
Some women have an amniocentesis because of a problem seen on ultrasound (for example, an increased nuchal translucency measurement). Having normal chromosomes on amniocentesis will be reassuring, but it may be just one part of investigating your baby for possible problems. There may still be concerns of other conditions affecting the baby.
For example, the risk of heart defects is increased when the nuchal translucency measurement is very thick.
The doctor will discuss the need for any further tests with you. These tests may include a detailed 18-20 week morphology ultrasound and a fetal echocardiogram (a specialised heart ultrasound of the baby).